目的 总结原发性中枢神经系统淋巴瘤(PCNSL)非典型MRI影像学表现,以提高对非典型PCNSL影像诊断的正确率。方法 回顾性分析经穿刺或手术病理证实的25例原发性中枢神经系统淋巴瘤的MRI影像学表现,包括非典型的生长部位,非特异的MRI表现和强化方式。结果 25例中单发病灶者16例,多发病灶9例,病灶数共38个。不典型发生部位可见于鞍上、脑干、小脑半球和小脑蚓部、侧脑室、三脑室和第四脑室等等。病灶形态大小不一,表现形式多种多样,可呈类圆形、不规则形,团块状、结节状、斑片状、灶状或散在分布。1例病灶
原发性中枢神经系统淋巴瘤非典型MRI影像学表现
赵 凯1) 张 岚2)△ 顾志强3)
1) 安阳市第六人民医院放射科,河南 安阳 455000 2) 河南中医药大学第一附属医院磁共振科,河南 郑州 450000 3)郑州大学第二附属医院放射科,河南 郑州 450014
作者简介:赵凯,Email:zhaokai9828@163.com
△通信作者:张岚,Email:13837187787@163.com
【摘要】 目的 总结原发性中枢神经系统淋巴瘤(PCNSL)非典型MRI影像学表现,以提高对非典型PCNSL影像诊断的正确率。方法 回顾性分析经穿刺或手术病理证实的25例原发性中枢神经系统淋巴瘤的MRI影像学表现,包括非典型的生长部位,非特异的MRI表现和强化方式。结果 25例中单发病灶者16例,多发病灶9例,病灶数共38个。不典型发生部位可见于鞍上、脑干、小脑半球和小脑蚓部、侧脑室、三脑室和第四脑室等等。病灶形态大小不一,表现形式多种多样,可呈类圆形、不规则形,团块状、结节状、斑片状、灶状或散在分布。1例病灶侵及邻近脑膜,出现“脑膜尾征”。20例在T1WI呈稍低或等信号,T2WI呈等或稍高信号,5例T1WI、T2WI呈混杂信号。7例呈实性均质强化,6例呈结节状强化,3例呈斑片状强化,2例呈条纹状强化,2例呈环形强化,1例呈弥漫肿胀伴轻度强化,3例多发病灶多种强化方式并存。5例DWI呈均质高信号,6例呈不均匀稍高信号,4例呈中等信号。MRS检查4例出现较明显的Lip峰。结论 对于发生在非典型生长部位、影像学表现非特异性的,以及颅内多发病灶的和侵犯脑膜的中枢神经系统淋巴瘤,术前诊断较为困难,需引起高度重视。
【关键词】 原发性中枢神经系统淋巴瘤;非典型;磁共振成像;立体定向穿刺活检;鉴别诊断
【中图分类号】 R739.41 【文献标识码】 A 【文章编号】 1673-5110(2018)19-2158-07 DOI:10.12083/SYSJ.2018.19.469
Atypical MRI manifestations of primary central nervous system lymphoma
ZHAO Kai1),ZHANG Lan2),GU Zhiqiang3)
1)Department of Radiology,Anyang People's Hospital NO.6,AnYang 455000,China;2)Vice-Director of MRI,the First Affiliated Hospital of Henan Medical University of TCM,Zhengzhou 450000,China;3)Department of Radiology,Second Affiliated Hospital of Zhengzhou University,Zhengzhou 450014,China
【Abstract】 Objective To summarize the atypical MRI manifestation of primary central nervous system lymphoma (PCNSL) in order to improve the correct diagnosis of PCNSL.Methods MRI imaging findings of 25 primary central nervous system lymphomas confirmed by puncture or surgical pathology were retrospectively analyzed,including atypical growth sites,non-specific MRI findings,and enhancement patterns.Results There were 38 lesions,including solitary lesion in 16 cases and multiple lesions in 9 cases.The atypical locations included sellar,pontine,cerebellum and cerebellar vermis,lateral ventricle,third and fourth ventricle,et al.The lesions demonstrated variously in size and appearance with oval-like,irregular,crumby,nodular,patchy and focal or diffuse shapes.One tumor invaded adjacent meninges with “meningeal tail sign”.The tumor showed low or iso-signal on T1WI and iso-or high signal on T2WI in 20 cases,and miscellaneous signals on T1WI and T2WI in 5 cases.The tumor showed homogeneous enhancement in 7 cases,nodular enhancement in 6 cases,patchy enhancement in 3 cases,stripe enhancement in 2 cases,rim enhancement in 1 case and slightly diffused enhancement in 1 case.The multiple lesions showed different enhancement patterns in 3 cases.The tumor showed homogeneous high signal on DWI in 5 cases,inhomogeneous slightly high signal on DWI in 6 cases,intermediate signal on DWI in 4 cases.There was an obvious Lip peak on MRS in 4 cases.Conclusion The preoperative diagnosis of PCNSL is difficult to make and should be paid great attention when the tumors occur in atypical locations with atypical and non-specific MRI features,and multiple lesions or involved meninges.
【Key words】 Primary central nervous system lymphoma;Atypical;Magnetic resonance imaging;Stereotactic needle biopsy;Differential diagnosis
原发性中枢神经系统淋巴瘤(primary central nervous system lymphoma,PCNSL)是指仅累及中枢神经系统,主要侵犯脑和脊髓的恶性非霍奇金淋巴瘤[1-5]。以往报道PCNSL多见于免疫功能异常的人群,如获得性免疫缺陷者(如AID、EB病毒感染)或长期服用免疫抑制剂的患者。随着对本病认识的不断加深,PCNSL在免疫功能正常的人群中发病率逐年提高[6-7]。PCNSL在颅内大多表现为大脑深部信号均匀的单发或多发病灶,肿瘤内出血、坏死、囊变和钙化少见,增强扫描通常明显均匀强化。但仍有部分病例表现不典型,极易误诊。本文通过回顾性分析25例经手术或穿刺病理证实的不典型PCNSL的影像学资料,分析其不典型发生部位、MRI表现等,以提高对非典型PCNSL诊断的正确率,为临床制定治疗方案提供依据[8-10]。
1 资料与方法
1.1 一般资料 搜集安阳市第六人民医院2013-01—2018-05经病理证实且术前误诊的PCNSL25例患者的资料,男18例,女7例,年龄26~78(56.8±11.2)岁。临床表现为颅高压症状如头痛、头晕、呕吐等;局部体征如肢体麻木、瘫痪、失语、共济失调等;认知和行为、精神改变。术前或穿刺前多误诊为转移瘤、胶质瘤、脑膜瘤、炎性脱髓鞘病变等。25例均经手术或立体定向穿刺活检病理证实。所有患者无先天性或获得性免疫功能缺陷病史,MRI检查前均未使用过激素治疗,并经骨髓细胞学或其他影像学检查(PET-CT)排除继发性淋巴瘤。
1.2 检查方法 采用西门子Verio 3.0T 超导型磁共振扫描机和头颈联合8通道线圈。扫描序列包括T1WI、T2WI和增强的轴位、冠状位和矢状位,以及弥散加权成像(diffusion weighted imaging,DWI)。层厚6 mm,层间距1 mm,视野(FOV) 230 mm×230 mm,矩阵384×384。T2WI:TR 6 000 ms,TE 90 ms;T1WI:TR 200 ms,TE 2.5 ms;FLAIR:TR 3 500 ms,TE 90 ms;DWI:TR 3 100 ms,TE 82 ms。增强扫描采用TSE序列,包括矢状位、冠状位、轴位。注射对比剂为Gd-DTPA(0.1 mmol/kg),注射流率为2 mL/s。扫描参数:TR 200 ms,TE 2.5 ms,层厚1 mm,层间距0。磁共振波谱成像(magnetic resonance spectroscopy,MRS) 检查采用多体素扫描,TR 1 600 ms,TE 125 ms,采集时间为8 min。在工作站进行MRS后处理,获得各代谢物分布曲线图。
1.3 手术或穿刺及病理 19 例行外科手术,6例行立体定向穿刺活检。10%甲醛溶液固定肿瘤组织,石蜡包埋,HE染色。光学显微镜下观察肿瘤细胞的分布密度、细胞核核浆比、血管分布及形态。
2 结果
2.1 病理结果 25例均诊断为PCNSL,其中19例为弥漫大B细胞淋巴瘤,3例为Burkitt淋巴瘤,2例为T细胞淋巴瘤,1例为黏膜相关性淋巴组织淋巴瘤。术前仅2例正确诊断为淋巴瘤,3例高度怀疑淋巴瘤,余误诊为转移瘤5例,胶质瘤7例,髓母细胞瘤1例,脑膜瘤1例,生殖细胞瘤1例,炎性脱髓鞘病变1例,不能定性者4例。镜下示肿瘤细胞异型明显,细胞核核浆比大,肿瘤细胞围绕正常血管呈套袖样浸润,肿瘤新生血管较少。
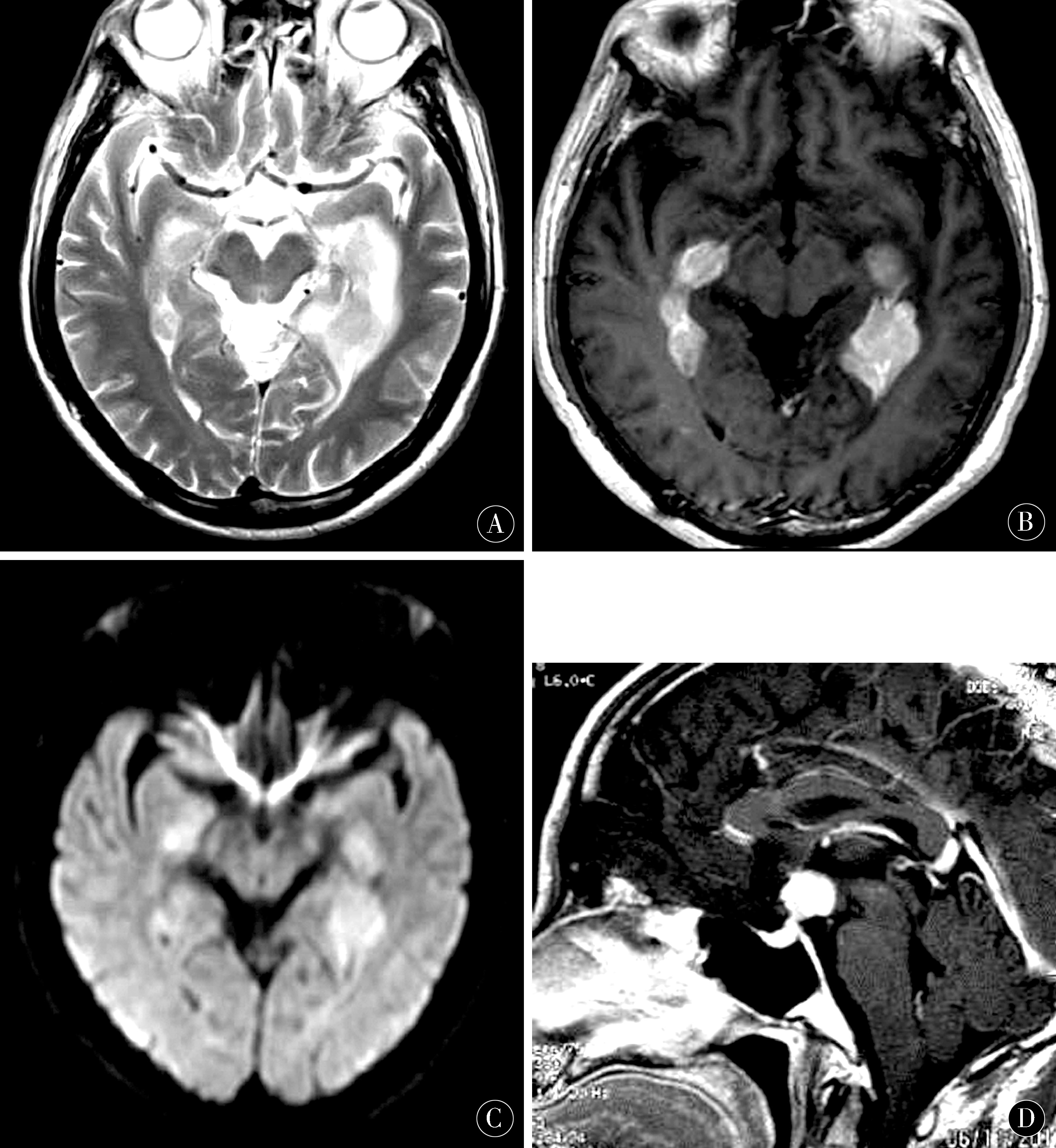
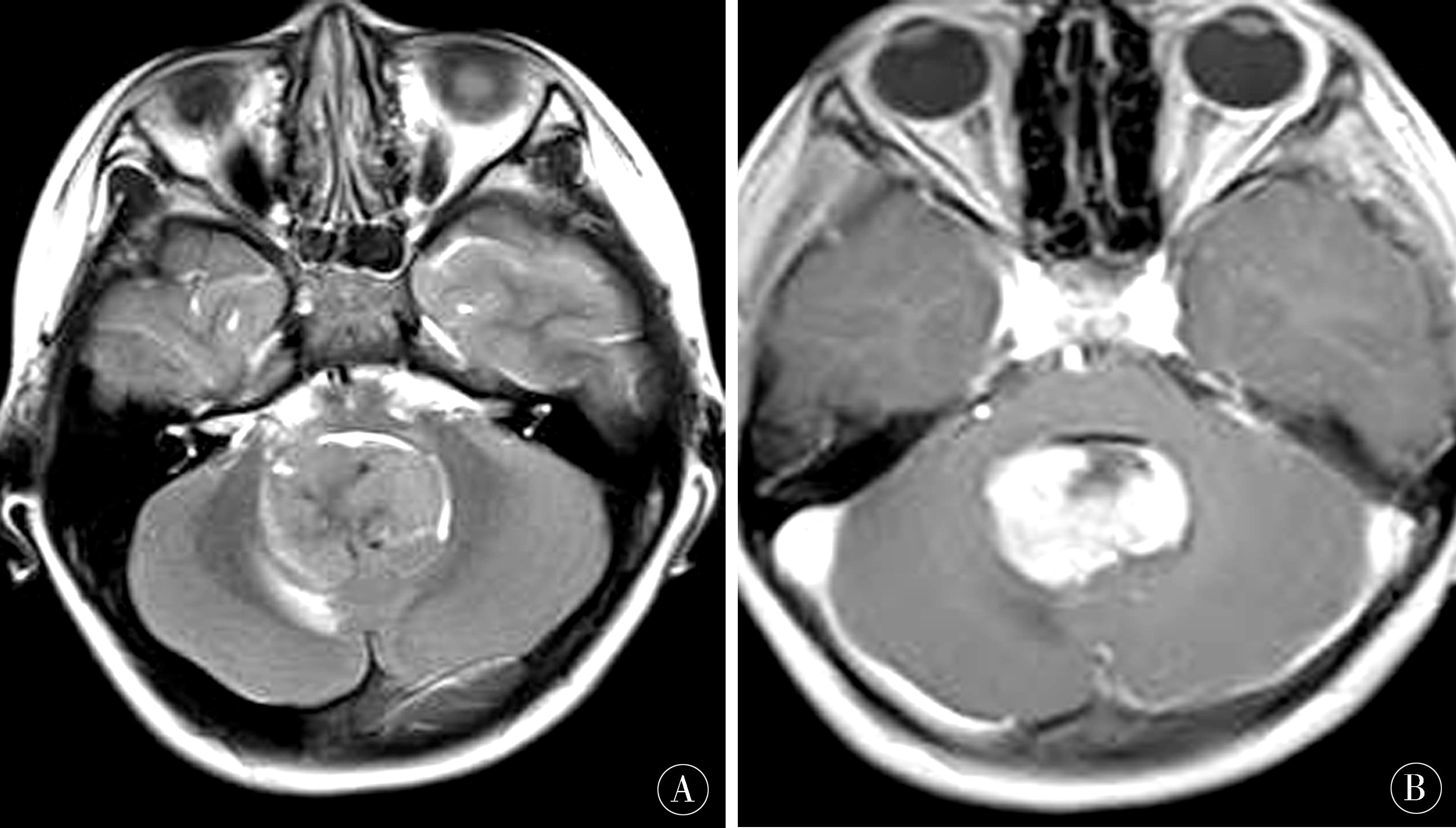
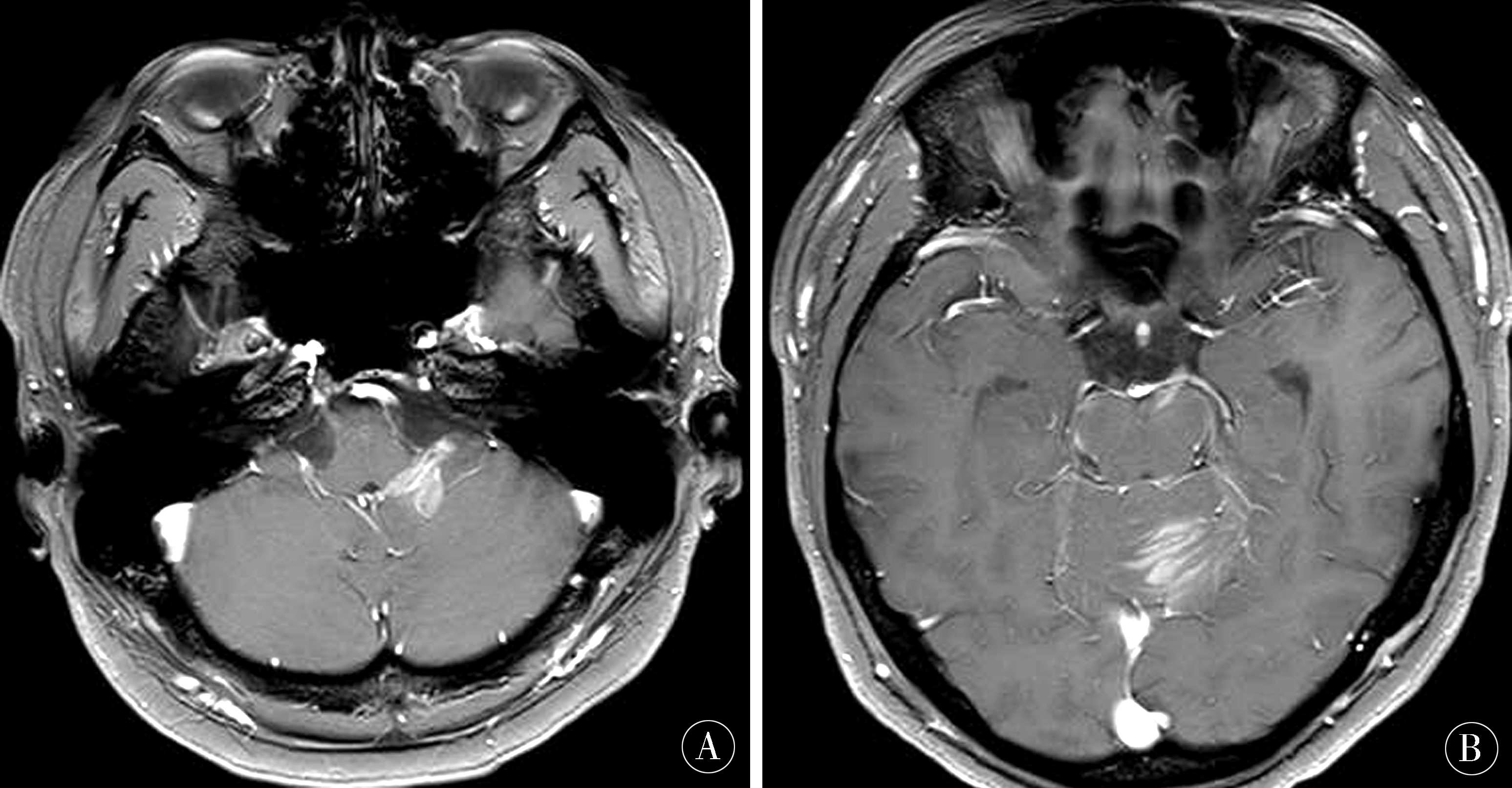
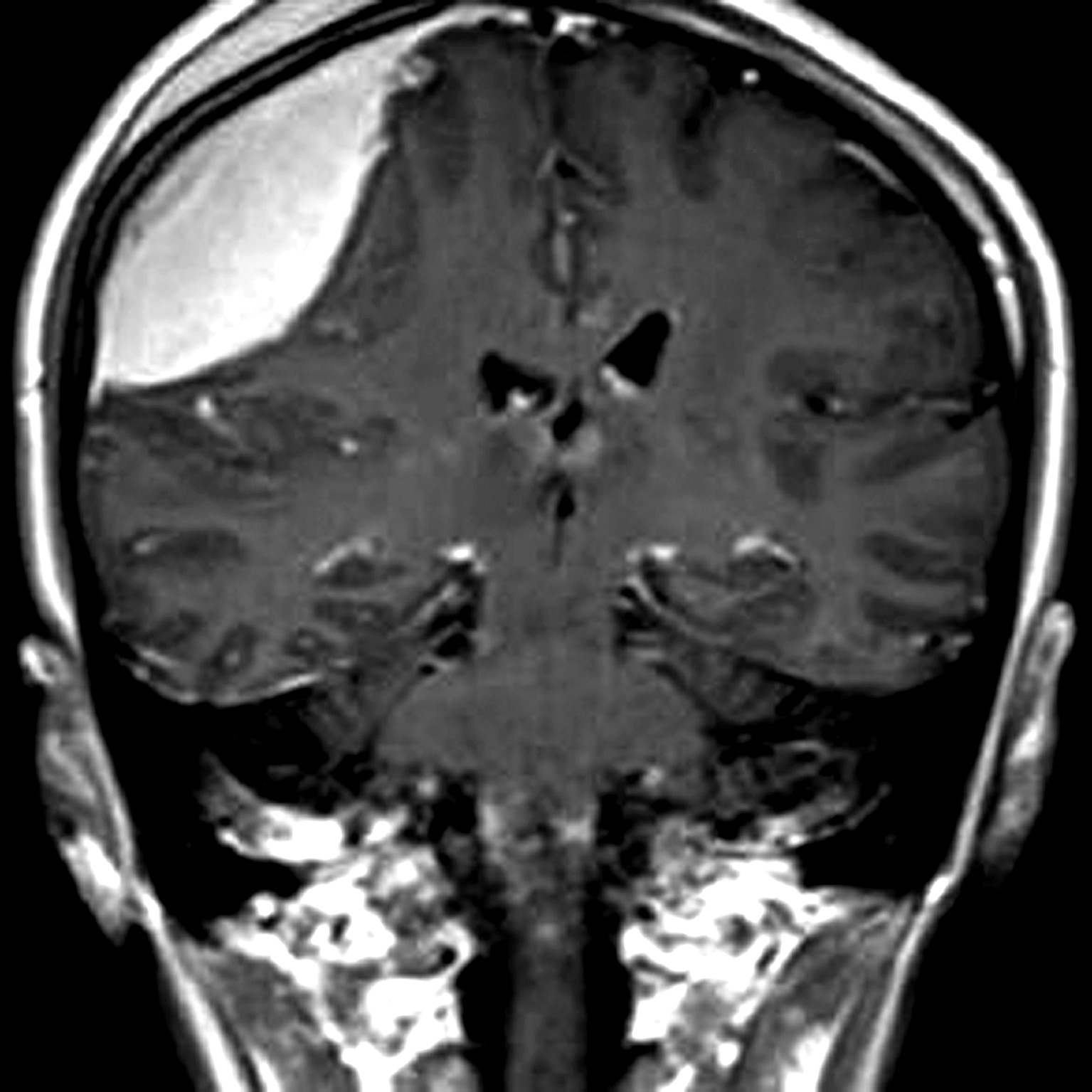
2.2 MRI表现 25例中单发病灶者16例,9例为多发病灶,4例多发病灶均位于幕上,3例幕上与幕下均发现病灶,2例多发病灶均位于幕下,病灶数共38个。38个病灶中,位于侧脑室和三脑室2个(图1),鞍上1个(图1),第四脑室1个(图2),脑干2个,小脑半球和小脑蚓部8个(图3),桥小脑角区1个,基底节区和丘脑3个,额叶灰白质交界区8个,颞叶灰白质交界区6个,颞枕叶皮层下3个,胼胝体3个。病灶形态大小不一,表现形式多种多样,可呈类圆形、不规则形,团块状、结节状、斑片状、灶状或散在分布。16 例病灶周围出现不同程度水肿。20例边界较为清晰,5例边界欠清晰; 1例病灶侵及邻近脑膜,引起脑膜增厚,并出现“脑膜尾征”(图4)。11例T1WI和T2WI均呈等信号,6例T1WI呈稍低信号、T2WI呈稍高信号,5例T1WI、T2WI呈混杂信号,3例T1WI呈等信号、T2WI呈高信号。增强扫描后,6例呈结节状强化(图1B,图1D),7例呈实性均匀强化(图4),3例呈斑片状强化(图3A),2例呈条纹状强化(图3B),2例呈环形强化,1例呈弥漫肿胀伴轻度强化。9例多发病灶中3例多种强化方式并存,结节状与片状强化同时存在,或实性均匀强化与环状强化同时存在。15例行DWI检查的患者中,5例呈均质高信号(图1C),6例呈不均匀稍高信号,4例呈中等信号。6例行MRS检查的患者中,4例在1.33 ppm 处出现较明显的Lip峰,余2例未见到Lip峰。
图1 男 65岁,弥漫大B细胞淋巴瘤。平扫轴位T2WI(A)、增强T1WI(B)、DWI(C)示双侧侧脑室旁颞角多发结节状T2WI稍高信号,增强扫描明显均匀强化,DWI呈均匀高信号(D)男,53岁,鞍上淋巴瘤,增强矢状位示鞍上异常强化结节
Figure 1 Male 65 years old,diffuse large B-cell lymphoma. The plain axial position T2WI(A),enhanced T1WI(B),and DWI(C) showed multiple nodular T2WI signals on both sides of the lateral ventricle,and the enhanced scan was uniform. Enhanced,DWI is a uniform high signal;(D) Male,53 years old,saddle lymphoma. Enhance the sagittal position to show abnormally enhanced nodules on the saddle
图2 男,6岁,Burkitt淋巴瘤。平扫轴位T2WI(A)、增强T1WI(B)示第四脑室中等信号肿块,肿块内裂隙样低信号,增强扫描明显异常强化,肿块内片状不强化区
Figure 2 Male,6 years old,Burkitt lymphoma. The plain axial position T2WI(A) and enhanced T1WI(B) showed a moderate signal mass in the fourth ventricle,a low-signal-like signal in the mass,an enhanced abnormal enhancement in the enhanced scan,and no plaque in the mass. Strengthened area
图3 男,29岁,Burkitt淋巴瘤。轴位增强T1WI(A、B) 示左侧小脑半球四脑室旁、小脑蚓部斑片状、条纹状异常强化
Figure 3 Male,29 years old,Burkitt lymphoma. Axial position enhancement T1WI(A, B) shows left cerebral hemispheres in the fourth ventricle, cerebellar verrucous patchy,streak-like abnormal enhancement
图4 女,28岁,黏膜相关性淋巴组织淋巴瘤。冠状位增强T1WI示右侧额部凸透镜形均匀强化病灶,伴脑膜尾征
Figure 4 Prostitute,28 years old,mucosa-associated lymphoid tissue lymphoma. Coronal enhancement T1WI showed a right frontal convex lens-shaped uniform enhancement lesion with meningeal tail sign
3 讨论
本组25例PCNSL的非典型MRI表现主要分为以下几类:(1) 非典型生长部位。PCNSL好发于幕上,如大脑深部近中线区,额叶、脑室周围,胼胝体、且易跨越中线生长。本组25例中,PCNSL可见于鞍上、基底节区、丘脑、灰白质交界区、侧脑室、脑干、小脑半球、小脑蚓部和侧脑室、第三、四脑室等。且多发病灶者可同时生长于大脑半球两侧,也可同时累及大脑半球和小脑,或呈弥漫性分布。本组1例发生在鞍上,1例为第四脑室单发肿瘤,1例为多发病灶位于小脑半球、小脑蚓部和中脑,术前均未能诊断正确。通常认为,PCNSL少见部位发病多见于免疫功能缺陷的人群,尤其是艾滋病患者[11-13],但本组所有患者无先天性免疫功能障碍或获得性免疫功能缺陷的病史及临床表现。(2) 多发病灶及散在分布的病灶。PCNL表现为多发病灶并不在少数,影像学表现为多中心浸润,可同时位于大脑半球的一侧或两侧,浅表区域和深部同时发病,或同时发生于大脑半球和小脑半球。本组中4例病灶为幕上、幕下散在分布,病变累及大脑深部和小脑半球,病灶大小、形态不一,增强后以实性强化为主,术前均诊断为转移瘤。本组1例为小脑半球、小脑蚓部和中脑多发病灶,增强后呈结节状、条纹状及片状强化,早期诊断为炎性脱髓鞘病变,且激素治疗后无效,后经立体定向穿刺活检确诊为PCNL。(3) 非典型MRI增强表现。典型的PCNSL增强扫描在免疫功能缺陷患者多呈环形强化;在免疫功能正常的患者多为类圆形或椭圆形肿块并呈明显均质强化,有时能见到一些典型强化征象,如 “握拳征”、“尖角征”、“脐凹征”等[14]。此特征性表现可能与肿瘤生长过快,生长过程中遇到较大血管阻挡有关[15-19]。但本组PCNSL中表现为肿块型的,增强后可见“脐凹征”,累及胼胝体的病灶可见“蝶翼征”;未表现为肿块形状的肿瘤,增强后可呈结节样强化、灶状强化、条纹状强化、斑片状强化等,或同一病例颅内多发病灶可以表现为不同的强化方式和强化程度。文献报道,无免疫功能缺陷的患者PCNSL增强后可表现为无强化,与经激素治疗后的PCNSL表现相似,早期诊断非常困难[20-21]。但本组病例未见到增强后无强化的病灶,所有病灶均有不同程度的强化,少部分病灶强化微弱但仍有强化。PCNSL周围可无水肿,也可出现水肿,多认为由于肿瘤周围血管浸润性生长导致血脑屏障的破坏引起的间质性水肿[22-25]。本组中16例病灶周围出现水肿,水肿程度不一。(4) 非典型DWI表现:由于肿瘤细胞构成密集,胞质少,核质比高,且肿瘤细胞外间隙小,含水量少,PCNSL中水分子扩散往往是受限的,因此DWI上呈高信号,ADC 图上为低信号[26-30]。单发肿块在DWI应表现为均质高信号。但本组病例部分肿块型的PCNSL在DWI上呈不均质中等信号,病灶内点片状低信号;而非肿块型的病灶多为稍高信号,或中心低信号为主的中等信号。(5)伴发脑膜改变。当淋巴瘤累及脑膜时,沿着相邻脑膜生长延伸并致其增厚强化,与脑膜瘤不易鉴别。
非典型的PCNSL MRI表现和颅内很多肿瘤表现类似,不易鉴别。其中多发非肿块型病灶和炎性脱髓鞘病变不易鉴别,早期诊断较为困难,且使用激素治疗可能会延误对淋巴瘤的正确判断。大脑深部累及胼胝体、跨越中线的淋巴瘤和胶质母细胞瘤有时难以鉴别[31-32]。弥漫浸润型淋巴瘤可累及大脑深部、深部灰质核团和灰白质交界区,此淋巴瘤表现与大脑胶质瘤病近似。淋巴瘤侵及脑膜时也可出现“脑膜尾征”,与脑膜瘤鉴别困难,但CT骨窗对显示颅骨的变化可能有助于二者鉴别[33-34]。当PCNSL表现为多发肿块时,需与转移瘤鉴别。转移瘤可有原发病史,增强后多为环形强化,且瘤体和瘤周水肿不成比例,“小肿瘤大水肿”的表现可能有助于鉴别。MRS对鉴别淋巴瘤与其他实性肿瘤具有高度特异性,当出现宽大的Lip峰可以作为淋巴瘤的特征性表现[35-37]。但本组病例行MRS检查的6例,仅有4例出现Lip峰,另外2例未见到Lip峰,考虑可能由于感兴趣容积(VOI)的选择和勾画不够精确所致。虽然MRS提示Lip峰,但仍有2例因为其发生部位和强化方式的不典型和不特异未能在术前诊断为PCNSL[38-40]。其他病例为多发病灶的尤其表现为斑片状和结节状的病灶,对其勾画VOI进行MRS检查较为困难。
本组病例不能涵盖所有中枢神经系统淋巴瘤的非典型和非特异表现,对于文献报道的增强后无强化的PCNSL本组病例并不包括。对于发生在非典型生长部位、影像学表现非特异性的,以及颅内多发病灶的和侵犯脑膜的中枢神经系统淋巴瘤,临床易误诊为其他恶性或良性肿瘤,甚至非肿瘤病变,早期诊断极为困难,需引起临床高度重视,最终均需靠立体定向穿刺活检或外科手术病理证实。
4 参考文献
[1] 王亮亮,王敏,王德杭.多模态MRI对原发性中枢神经系统淋巴瘤的诊断价值[J].医学影像学杂志,2016,26(8):1 379-1 383.
[2] 李连霞,张延军,崔阿娜,等.磁共振成像在颅内原发性中枢神经系统淋巴瘤诊断中应用研究[J].影像研究与医学应用,2018,2(6):54-55.
[3] 蔡东梅.原发性中枢神经系统淋巴瘤的磁共振成像的影像诊断及病理特点[J].实用医学影像杂志,2018,19(2):176-177.
[4] 张建,李晶.磁共振成像在原发性中枢神经系统淋巴瘤诊断中的应用价值[J].新疆医学,2016,46(10):1 287-1 290.
[5] 景治涛,崔启韬,李连翔,等.原发性中枢神经系统淋巴瘤 CT 、M RI 表现及临床病理特征[J].陕西医学杂志,2016,45(6):690-692.
[6] MATSUMOTO Y,KASHIMURA H,ASO K,et al.Primary centralnervous system lymphoma presenting as growing intracerebral hemorrhage[J].World Neuros-urg,2018,23.pii:S1878-8750(18)31060-X.doi:10.1016/j.wneu.2018.05.107.
[7] KUNIMATSU A,KUNIMATSU N,YASAKA K,et al.Machine Learning-based Texture Analysis of Contrast-enhanced MR Imaging to Differentiate between Glioblastoma and Primary Central Nervous System Lymphoma[J].Magn Reson Med Sci,2018,16.doi:10.2463/mrms.mp.2017-0178.
[8] LI M G,CHEN Z Y,LIU G,et al.Value of Minimum Apparent Diffusion Coefficient in Peritumoral Edema in the Differential Diagnosis between Primary Central Nervous System Lymphoma and Glioblastoma[J].Zhongguo Yi Xue Ke Xue Yuan Xue Bao,2018,40(2):146-150.
[9] SUH H B,CHOI Y S,BAE S,et al.Primary central nervous system lymphoma and atypical glioblastoma:Differentiation using radiomics approach[J].Eur Radiol,2018,6.doi:10.1007/s00330-018-5368-4.
[10] MALIKOVA H,BURGHARDTOVA M,KOUBSKA E,et al.Secondary central nervous system lymphoma:spectrum of morphological MRI appearances[J].Neuropsychiatr Dis Treat,2018,14:733-740.
[11] ERDAG N,BHORADE R M,ALBERICO R A,et al.Primary lymphoma of the central nervous system:typical and atypical CT and MR imaging appearances[J].AJR Am J Roentgenol,2001,176(5):1 319-1 326.
[12] WU Y,DEN Z,LIN Y.Accuracy of Susceptibility-Weighted Imaging and DynamicSusceptibility Contrast Magnetic Resonance Imaging for Differentiating High-GradeGlioma from Primary Central Nervous System Lymphomas:Meta-Analysis[J].World Neurosurg,2018,112:e617-e623.
[13] NESKA-MATUSZEWSKA M,BLADOWSKA J,SASIADEK M,et al.Differentiation ofglioblastoma multiforme,metastases and primary central nervous system lymphomasusing multiparametric perfusion and diffusion MR imaging of a tumor core and aperitumoral zone-Searching for a practical approach[J].PLoS One,2018,13(1):e0191341.
[14] 吴春梅,邹艳,康庄,等.MRI 表现非典型的原发性中枢神经系统淋巴瘤三例[J].新医学,2015(3):190-195.
[15] 冯洁,叶勇军,舒恩芬.原发性中枢神经系统淋巴瘤的MRI诊断及病理特点分析[J].医学影像学杂志,2017,27(12):2 404-2 407.
[16] 全国彪,张康胜,周伟文,等.原发性中枢神经系统T细胞淋巴瘤的磁共振成像特征研究[J].中国CT和MRI杂志,2018,16(1):36-39.
[17] 耿磊,孙毅,孙志先,等.MRI鉴别诊断原发性中枢神经系统淋巴瘤与高级别胶质瘤深部病灶[J].中国介入影像与治疗学,2018,15(2):95-99.
[18] 林洪平,肖大春,邵晓彤,等.原发性中枢神经系统淋巴瘤的MRI特征分析[J].实用放射学杂志,2018,34(3):347-350.
[19] 苗炜宇,张岚. 磁共振弥散加权成像在鉴别脑内淋巴瘤与高级别胶质瘤中的应用价值[J].中国实用神经病杂志,2016,19(8):65-67.
[20] 张秀苓,史长虹.CT、MRI多模态检查对颅内原发性中枢神经系统淋巴瘤的诊断价值[J].中国中西医结合影像学杂志,2018,16(1):15-17;25.
[21] 何毅华,杨新光,龙友明,等.原发性中枢神经系统淋巴瘤的不典型MRI表现[J].齐齐哈尔医学院学报,2017,38(12):1 377-1 381.
[22] 董安珂,张勇,程敬亮.等.后颅窝原发性中枢神经系统淋巴瘤的磁共振多模态诊断[J].临床放射学杂志,2016,35(9):1 303-1 307.
[23] CHEN Y,LI Z,WU G,et al.Primary central nervous system lymphoma and glioblastoma differentiation based on conventional magneticresonance imaging by high-throughput SIFT features[J].Int J Neurosci,2018,128(7):608-618.
[24] NAGASHIMA H,SASAYAMA T,TANAKA K,et al.Myo-inositolconcentration in MR spectroscopy for differentiating high grade glioma fromprimary central nervous system lymphoma[J].J Neurooncol,2018,136(2):317-326.
[25] MAKINO K,HIRAI T,NAKAMURA H,et al.Differentiating Between Primary Central Nervous System Lymphomas and Glioblastomas:Combined Use of Perfusion-Weighted and Diffusion-Weighted Magnetic Resonance Imaging[J].World Neurosurg,2018,112:e1-e6.
[26] OZDEMIR E S,YILDIRIM A E,CAN A Y.Primary Central Nervous System Lymphoma ofOptic Chiasma:Endoscopic Endonasal Treatment[J].J Craniofac Surg,2018,29(1):199-201.
[27] YU H,GAO B,LIU J,et al.Lymphomatosis cerebri:a rare variant of primary central nervous system lymphoma and MR imaging features[J].Cancer Imaging,2017,17(1):26.
[28] AHLE G,TOUITOU V,CASSOUX N,et al.Optic Nerve Infiltration in Primary Central Nervous System Lymphoma[J].JAMA Neurol,2017,74(11):1 368-1 373.
[29] LU S,WANG S,GAO Q,et al.Quantitative Evaluation of Diffusion and Dynamic Contrast-Enhanced Magnetic Resonance Imaging for Differentiation Between Primary Central Nervous System Lymphoma and Glioblastoma[J].J Comput Assist Tomogr,2017,41(6):898-903.
[30] WEN J B,HUANG W Y,XU W X,et al.Differentia-ting PrimaryCentral Nervous System Lymphomas From Glioblastomas and InflammatoryDemyelinating Pseudotumor Using Relative Minimum Apparent Diffusion Coefficients[J].J Comput Assist Tomogr,2017,41(6):904-909.
[31] KUNIMATSU A,KUNIMATSU N,KAMIYA K,et al.Comparison between Glioblastoma and Primary Central Nervous System Lymphoma Using MR Image-based Texture Analysis[J].Magn Reson Med Sci,2018,17(1):50-57.
[32] ALCAIDE-LEON P,DUFORT P,GERALDO A F,et al.Differentiation of Enhancing Glioma and Primary Central Nervous System Lymphoma by Texture-Based Machine Learning[J].AJNR Am J Neuroradiol,2017,38(6):1 145-1 150.
[33] XU W,WANG Q,SHAO A,et al.The performance of MR perfusion-weightedimaging for the differentiation of high-grade glioma from primary central nervoussystem lymphoma:A systematic review and meta-analysis[J].PLoS One,2017,12(3):e0173430.
[34] ALESSANDRO L,PASTOR RUEDA J M,VILLALONGA J F,et al.Retrospective study of 48 cases of primary central nervous system lymphoma.Medicina (B Aires),2017,77(1):17-23.
[35] ZHAO Q,ZENG L S,FENG X L,et al.Magnetic Resonance ImagingCharacteristics of Primary Central Nervous System T-cell Lymphoma[J].Chin Med J(Engl),2017,130(3):374-376.
[36] FOSSARD G,FERLAY C,NICOLAS-VIRELIZIER E,et al.Utility of post-therapy brain surveillance imaging in the detection of primary central nervous system lymphoma relapse[J].Eur J Cancer,2017,72:12-19.
[37] KOUBSKA E,WEICHET J,MALIKOVA H.Central nervous system lymphoma:amorphological MRI study[J].Neuro Endocrinol Lett,2016,37(4):318-324.
[38] EVERS G,KAMP M,WARNEKE N,et al.5-Aminolaevulinic Acid-Induced Fluorescence in Primary Central Nervous System Lymphoma[J].World Neurosurg,2017,98:375-380.
[39] LU S,GAO Q,YU J,et al.Utility of dynamic contrast-enhanced magnetic resonance imaging for differentia-ting glioblastoma,primary central nervous system lymphoma and brain metastatic tumor[J].Eur J Radiol,2016,85(10):1 722-1 727.
[40] JIMÉNEZ D E L A,PEA M D,VICENTE L G,et al.The Multiple Faces of Nervous System Lymphoma.Atypical Magnetic Resonance Imaging Features and Contribution of the Advanced Imaging[J].Curr Probl Diagn Radiol,2017,46(2):136-145.
(收稿2018-06-10 修回2018-07-10)
本文责编:关慧
本文引用信息:赵凯,张岚,顾志强.原发性中枢神经系统淋巴瘤非典型MRI影像学表现[J].中国实用神经疾病杂志,2018,21(19):2158-2164.DOI:10.12083/SYSJ.2018.19.469
Reference information:ZHAO Kai,ZHANG Lan,GU Zhiqiang.Atypical MRI manifestations of primary central nervous system lymphoma[J].Chinese Journal of Practical Nervous Diseases,2018,21(19):2158-2164.DOI:10.12083/SYSJ.2018.19.469