目的 探讨3D-TOF-MRA多模式成像在面肌痉挛显微血管减压术中的价值。方法 49例面肌痉挛病人用1.5T磁共振机行3D-TOF序列轴位扫描,实验组为神经外科手术医师在影像工作站分别用多平面重建、最大信号强度投影、透明化彩色容积再现等成像模式及合适的成像参数,进行多层面多角度观察,诊断神经血管压迫点及责任血管。对照组为在PACS工作站的诊断结果。以手术所见为金标准,计算2组诊断符合率。结果 49例均在术中发现责任血管及明确压迫点,实验组压迫点诊断符合率83.7%,对照组51.0%,2组比较差异有统计学意义(P<0.05)。实验组责任血管诊断符合率81.6%,对照组65.3%,2组比较差异有统计学意义(P<0.05)。结论 神经外科手术医师在影像工作站行3D-TOF-MRA多模式成像,对面肌痉挛病人神经血管压迫点和责任血管的诊断符合率优于在PACS工作站诊断。
3D-TOF-MRA多模式成像在面肌痉挛显微血管减压术中的价值
张长远
河南省人民医院神经外科,河南 郑州 450003
作者简介:张长远,Email:zcy153@163.com
【摘要】 目的 探讨3D-TOF-MRA多模式成像在面肌痉挛显微血管减压术中的价值。方法 49例面肌痉挛病人用1.5T磁共振机行3D-TOF序列轴位扫描,实验组为神经外科手术医师在影像工作站分别用多平面重建、最大信号强度投影、透明化彩色容积再现等成像模式及合适的成像参数,进行多层面多角度观察,诊断神经血管压迫点及责任血管。对照组为在PACS工作站的诊断结果。以手术所见为金标准,计算2组诊断符合率。结果 49例均在术中发现责任血管及明确压迫点,实验组压迫点诊断符合率83.7%,对照组51.0%,2组比较差异有统计学意义(P<0.05)。实验组责任血管诊断符合率81.6%,对照组65.3%,2组比较差异有统计学意义(P<0.05)。结论 神经外科手术医师在影像工作站行3D-TOF-MRA多模式成像,对面肌痉挛病人神经血管压迫点和责任血管的诊断符合率优于在PACS工作站诊断。
【关键词】 面肌痉挛;显微血管减压术;责任血管;3D-TOF-MRA;神经血管压迫点
【中图分类号】 R745.1+1 【文献标识码】 A 【文章编号】 1673-5110(2019)02-0159-05 DOI:10.12083/SYSJ.2019.02.031
Value of 3D-TOF-MRA multimode imaging for microvascular decompression of hemifacial spasm
ZHANG Changyuan
Department of Neurosurgery,Henan Provincial People's Hospital,Zhengzhou 450003,China
【Abstract】 Objective To explore the value of multi-mode 3D-TOF-MRA imaging for microvascular decompression of hemifacial spasm.Methods 49 cases of hemifacial spasm underwent 3D-TOF axial scan with 1.5T magnetic resonance machine.The experimental group underwent multiplane reconstruction,maximum intensity projection,transparent color volume rendering with appropriate imaging parameters at the imaging workstation.Multilayer and multi-direction observation was performed by neurosurgeons to diagnose neurovascular compression points and offending vessels.The control group was diagnosed at PACS workstation.The diagnostic coincidence rate of the two groups was calculated according to the intraoperative findings.Results The offending vessels and compression points were found in 49 cases.The diagnostic coincidence rate of compression points was 83.7% in the experimental group and 51.0% in the control group with significant difference (P<0.05).The diagnostic coincidence rate of the offending vessels was 81.6% in the experimental group and 65.3% in the control group with significant difference (P<0.05).Conclusion It is better that neurosurgeons perform 3D-TOF-MRA multi-modality imaging on imaging workstation to judge neurovascular compression points and offending vessels in patients with hemifacial spasm than that on PACS workstation.
【Key words】 Hemifacial spasm;Microvascular decompression;Offending vessels;3D-TOF-MRA;Neurovascular compression point
显微血管减压术(microvascular decompression,MVD)是治疗面肌痉挛的有效方法[1-3]。神经血管压迫点和责任血管的术前准确诊断对手术有积极的指导作用[4-5]。本研究应用3D-TOF序列对面肌痉挛病人进行术前轴位扫描,结合后处理技术多模式成像,显示造成压迫的责任血管,并与术中所见进行对比。
1 资料与方法
1.1 一般资料 选取2016-01—2017-08临床诊断为原发性面肌痉挛并手术者49例,男20例,女29例,年龄35~70岁,平均48.2岁;病变位于左侧32例,右侧17例;病程6个月~10 a。
1.2 扫描方法 应用美国GE SIGNA HDe 1.5T MRI扫描仪和8通道头颈联合线圈。扫描范围从顶部到延髓下部,扫描角度与前后联合连线平行,3D-TOF序列轴位扫描参数:TR 27 ms,TE 3.9 ms,翻转角(flip angle,FA)20°,FOV 22 cm×20 cm,矩阵288×192,层厚1.4 mm,层间距0.7 mm,NEX=1。
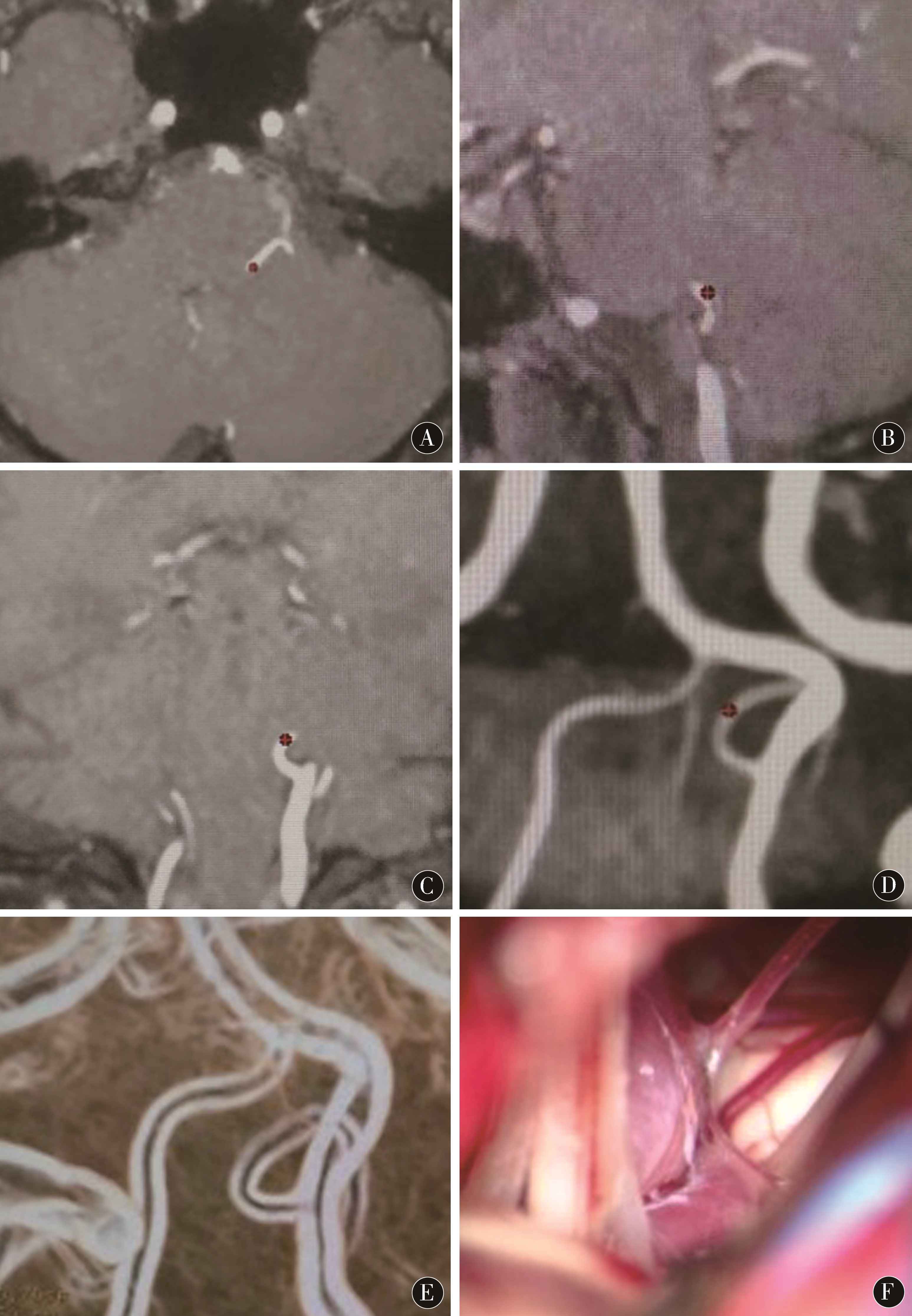
1.3 图像后处理及分析 将采集的3D-TOF-MRA原始图像传递至AV VolumeShare 2工作站。分别采用3D最大信号强度投影(maximum intensity projection,MIP)模式对原始图像进行血管重建(图1D),多平面重建模式(multi plane reconstruction,MPR)重建冠状位和矢状位图像(图1A~C),通过不断调整合适的层厚观察血管形态;然后用透明化Willis彩色容积再现(transparent Willis volume rendering,VR)模式成像,显示轮廓增强的血管(图1E),以立体的形式进行任意角度旋转。由神经外科手术医师和影像诊断医师共同观察面神经中枢段与邻近血管的关系,判断责任血管及压迫点,对手术可能操作到的血管走行进行详细分析诊断。
图1 左侧椎动脉发出的小脑后下动脉向内向上屈曲延长,在椎动脉背侧交叉反折向下走行,压迫点(※)在上橄榄窝 A:MPR模式轴位;B:矢状位;C:冠状位;D:MIP模式前面观不易确认血管前后关系;E:VR模式前面观更容易确认血管前后关系;F:术中照片见椎动脉压在小脑后下动脉上,血管脑干压迫点在更内侧
Figure 1 The posterior inferior cerebellar artery arising from the left vertebral artery is flexed inward and upward,and then turns downward across the vertebral artery posteriorly.The compression point (※) is in the upper olivary fossa.A:MPR mode axial section;B:Sagittal section;C:Coronal section;D:MIP mode is not easy to confirm the vascular's anterior-posterior relationship;E:VR mode front view iseasier to confirm the vascular's relationship;F:Intraoperative photo shows the vertebral artery compressing on the posterior inferior cerebellar artery,and the vascular brainstem compression point being hided inside
1.4 对照组在工作站分析 图像前,由同一影像诊断医师将采集的3D-TOF-MRA原始图像、MIP血管重建图像、MPR重建图像通过PACS发送至医生站,同一神经外科手术医师对压迫点及责任血管作出诊断。
1.5 与手术结果对比 以MVD术中所见及术后两名富有经验的神经外科医师对手术录像中压迫点及相关血管的走行(图1F)分析判断为金标准,与术前2组影像诊断结果进行对比,评价诊断准确情况。
1.6 统计学分析 采用SPSS 22.0软件进行统计学分析,计数资料以例数或百分比表示,比较采用χ2检验,P<0.05为差异有统计学意义。
2 结果
49例术中发现责任血管及明确压迫点,手术顺利,无脑脊液漏及颅内感染。术后随访1 a以上,43例面部抽搐完全消失,6例偶有轻微抽搐,无复发;5例遗留轻微面瘫,5例持续轻微听力下降,1例术后24 h迟发小脑血肿,紧急行开颅血肿清除术救治成功,部分生活自理。术前对照组诊断出压迫点32例,不确定17例,与手术所见一致25例,总体符合率51.0%。对责任血管来源和走行的诊断32例符合,符合率65.3%。在工作站进行的多模式多层面多角度影像诊断确定压迫点43例,不确定6例,与手术所见一致41例,总体符合率83.7%。对责任血管来源和走行的诊断40例符合,符合率81.6%,对压迫点和责任血管的诊断符合率均高于对照组,差异有统计学意义(P<0.05)。
3 讨论
尽管原发性面肌痉挛的发病机制还有争议[6-7],但可以确定其是一种神经血管压迫性疾病[8-9]。MVD是目前治疗面肌痉挛的有效手段,但术后仍有一定的并发症和复发率[10-12]。复发原因主要是对责任血管辨别失误或遗漏,由于椎动脉参与压迫而减压不充分,Teflon棉放置过多造成新的压迫等[13-15]。面瘫和听力损伤的并发症则是因术中神经牵拉损伤、手术导致血管痉挛等[16-18]。因此,选择合适的磁共振成像序列以使神经血管的解剖关系得以清晰显示是MVD手术的关键[19-21]。术前通过影像学检查,需要对有无责任血管压迫、压迫点及相关血管的走行进行全面精确的诊断。这对于手术计划及手术操作会有很大的指导,对于提高面肌痉挛显微血管减压手术效果、减少创伤和并发症、缩短手术时间有很大的帮助。
面肌痉挛MVD术前通常行头部3D-TOF-MRA检查,由影像医师作出诊断并将原始图像、MIP血管重建图像、MPR重建图像通过PACS发送至医生站[22]。影像医师与手术医师缺乏沟通,手术医师查看图像时不能做3D旋转,因此,手术所需要的图像信息受限,无法作出准确的判断。单靠影像医生的报告描述术者同样无法做到“心中有数”。手术医师前移到影像工作站,利用有更多功能的专门的影像处理软件,对感兴趣血管进行多模式多平面多角度观察,可以获取MVD手术过程中需要的关于压迫点和责任血管的更全面准确的信息,为手术策略的制定提供指导。对原始轴位图像及MPR重建冠状位和矢状位图像各个层面的连续观察,可以准确确认压迫点、责任血管的来源及走行。MIP血管重建图像以及透明化Willis彩色VR模式成像有助于从整体上确定有无动脉瘤、动脉狭窄、椎基底动脉及责任血管是否扩张延长,帮助确定对相关血管的分离范围、抬起方向和Teflon棉放置顺序和厚度,有助于减少术中不必要的操作,有利于手术的微创化和精准化。
3D-FIESTA轴位薄层扫描和MPR冠状位、矢状位重建成像,对于面神经脑池段显示更清楚,并能显示血流速度较慢的小动脉分支和静脉血管,对显示血流速度较快的中等血管不如3D-TOF-MRA成像[23-24]。而面肌痉挛绝大多数是由于动脉血管压迫,静脉参与压迫者在面肌痉挛病人明显少于三叉神经痛,且绝大部分病例神经血管冲突点在脑干表面的近端,在TZ以远的脑池段很少见[25-26]。因此,面肌痉挛病人术前3D-TOF-MRA检查作用更大,对于3D-TOF-MRA检查阴性者可进一步行3D-FIESTA检查。基于多模态神经影像的虚拟现实技术对于神经和血管的关系显示更加直观形象[27-28],但目前尚不能普及。另外,因与三叉神经痛MVD需要全程探查减压不同,面肌痉挛MVD只需自听神经-舌咽神经连线向深部观察到桥延沟,位置较固定,所以只要对该部位血管进行针对性的减压操作即可,不涉及对神经的过多牵拉[29-30]。目前最广泛应用的1.5T磁共振机及影像工作站软件中应用最普及、操作最简单的是3D-TOF-MRA,因此,充分利用现有条件,通过多模式显示血管和脑干的关系及相关血管弯曲和走行,是最方便实用的选择。
3D-TOF-MRA多模式成像诊断结果与手术所见符合率高,但仍有部分局限,主要是因部分病人后颅窝容积小、蛛网膜增厚,在分离蛛网膜的过程中还没有看清压迫点就得到减压,或是静脉性压迫、小动脉压迫在磁共振图像上不能很好显示。对于3D-TOF-MRA多模式成像诊断明确的病例,对手术有很好的指导作用,对于多模式成像诊断压迫点和责任血管不明确的病例,往往术中容易发现和处理病变,因此总体手术效果较好。
4 参考文献
[1] LYU M Y,DENG S L,LONG X F,et al.Long-term outcome of microvascular decompression for hemifacial spasm[J].Br J Neurosurg,2017,31(3):322-326.
[2] BARKER NDF G,JANNETTA P J,BISSONETTED J,et al.Microvascular decompression for hemifacial spasm[J].J Craniofac Surg,2008,23(5):1 385-1 387.
[3] SINDOU M,ESQUEDALIQUIDANO M,BRINZEU A.Microvascular Decompression for Hemifacial Spasm[J].Neurosurgery,2015,23(5):1 385-1 387.
[4] OHTANI K,MASHIKO T,OGURO K,et al.Preoperative three-dimensional diagnosis of neurovascular relationships at the root exit zones during microvascular decompression for hemifacial spasm[J].World Neurosurg,2016,92(5):171-178.
[5] CHUNG S S,CHANG J W,KIM S H,et al.Microvascular Decompression of the Facial Nerve for the Treatment of Hemifacial Spasm:Preoperative Magnetic Resonance Imaging Related to Clinical Outcomes[J].Acta Neurochir,2000,142(8):901-907.
[6] WILKINSON M F,CHOWDHURY T,MUTCH W A,et al.Analysis of facial motor evoked potentials for assessing a central mechanism in hemifacial spasm[J].J Neurosurg,2017,126(2):1-7.
[7] LEFAUCHEUR J P.New insights into the pathophysiology of primary hemifacial spasm[J].Neuro Chir,2018,64(2):87-93.
[8] MILLER L E,MILLER V M.Safety and effectiveness of microvascular decompression for treatment of hemifacial spasm:a systematic review[J].Br J Neurosurg,2012,26(4):438-444.
[9] DOU N N,ZHONG J,ZHOU Q M,et al.The mechanism of hemifacial spasm:a new understanding of the offending artery[J].Neurol Res,2014,37(2):184-188.
[10] HYUN S J,KONG D S,PARK K.Microvascular decompression for treating hemifacial spasm:lessons learned from a prospective study of 1,174 operations[J].Neurosurg Rev,2010,33(3):325-334.
[11] MCLAUGHLIN M R,JANNETTA P J,CLYDE B L,et al.Microvascular decompression of cranial nerves:lessons learned after 4400 operations[J].J Neurosurg,1999,90(1):1-8.
[12] QI H,ZHANG W,ZHANG X,et al.Microvascular Decompression Surgery for Hemifacial Spasm[J].J Craniofac Surg,2015,10(5):563-566.
[13] JIANG C,WU X,DAI Y,et al.Failed microvascular decompression surgery for hemifacial spasm:a retrospective clinical study of reoperations[J].Acta Neurochir,2017,159(2):259-263.
[14] PARK Y S,CHANG J H,CHO J,et al.Reoperation for Persistent or Recurrent Hemifacial Spasm after Microvascular Decompression[J].Neurosurgery,2006,58(6):1 162-1 167.
[15] HATAYAMA T,KONO T,HARADA Y,et al.Indications and Timings of Re-operation for Residual or Recurrent Hemifacial Spasm after Microvascular Decompression:Personal Experience and Literature Review[J].Neurol Medicochir,2015,55(8):663-668.
[16] HUH R,HAN I,MOON J,et al.Microvascular decompression for hemifacial spasm:analyses of operative complications in 1582 consecutive patients[J].SurgNeurol,2008,69(2):153-157.
[17] DAI Y,NI H,XU W,et al.Clinical analysis of hemifacial spasm patients with delay symptom relief after microvascular decompression of distinct offending vessels[J].Acta Neurol Belg,2015,116(1):1-4.
[18] LEE M H,LEE H S,JEE T K,et al.Cerebellar retraction and hearing loss after microvascular decompres-sion for hemifacial spasm[J].Acta Neurochir,2015,157(2):337-343.
[19] DOLATI P,GOLBY A,EICHBERG D,et al.Pre-Operative Image-based Segmentation of the Cranial Nerves and Blood Vessels in Microvascular Decompression:Can we Prevent Unnecessary Explorations?[J].Clin Neurol Neurosurg,2015,139:159-165.
[20] OISHI M,FUKUDA M,HIRAISHI T,et al.Interactive virtual simulation using a 3D computer graphics model for microvascular decompression surgery[J].J Neurosurg,2012,17(3):555-565.
[21] HUGHES M A,BRANSTETTER B F,TAYLOR C T,et al.MRI findings in patients with a history of failed prior microvascular decompression for hemifacial spasm:how to image and where to look[J].Am J Neuroradio,2015,36(4):768-773.
[22] KUMON Y,SAKAKI S,KOHNO K,et al.Three-dimensional imaging for presentation of the causative vessels in patients with hemifacial spasm and trigeminal neuralgia[J].Surg Neurol,1997,47(2):178-184.
[23] OHTA M,KOBAYASHI M,WAKIYA K,et al.Preoperative assessment of hemifacial spasm by the coronal heavily T2-weighted MR cisternography[J].Acta Neurochir,2014,156(3):565-569.
[24] DONAHUE J H,ORNAN D A,MUKHERJEE S.Imaging of Vascular Compression Syndromes[J].Radiol Clin N Am,2017,55(1):123-138.
[25] ZHONG J,ZHU J,SUN H,et al.Microvascular decompression surgery:surgical principles and technical nuances based on 4000 cases[J].Neurol Res,2014,36(10):882-893.
[26] TODA H,IWASAKI K,YOSHIMOTO N,et al.Bridging veins and veins of the brainstem in microvascular decompression surgery for trigeminal neuralgia and hemifacial spasm[J].Neurosurg Focus,2018,45(1):E2.
[27] OISHI M,FUKUDA M,HIRAISHI T,et al.Interactive virtual simulation using a 3D computer graphics model for microvascular decompression surgery[J].J Neurosurg,2012,117(3):555-565.
[28] YAO S,ZHANG J,ZHAO Y,et al.Multimodal Image-based Virtual Reality Pre-surgical Simulation and Evaluation for Trigeminal Neuralgia and Hemifacial Spasm[J].World Neurosurg,2018,113:e409-e507.
[29] IIJIMA K,HORIGUCHI K,YOSHIMOTO Y.Microvascular decompression of the root emerging zone for hemifacial spasm:evaluation by fusion magnetic resonance imaging and technical considerations[J].Acta Neurochir,2013,155(5):855-862.
[30] SINDOU M,MERCIER P.Microvascular decompres-sion for hemifacial spasm:Surgical techniques and intraoperative monitoring[J].Neuro Chir,2018,64(2):133-143.
(收稿2018-10-18)
本文责编:夏保军
本文引用信息:张长远.3D-TOF-MRA多模式成像在面肌痉挛显微血管减压术中的价值[J].中国实用神经疾病杂志,2019,22(2):159-163.DOI:10.12083/SYSJ.2019.02.031
Reference information:ZHANG Changyuan.Value of 3D-TOF-MRA multimode imaging for microvascular decompression of hemifacial spasm[J].Chinese Journal of Practical Nervous Diseases,2019,22(2):159-163.DOI:10.12083/SYSJ.2019.02.031